FAQ's and Forms
Frequently Asked Questions about
Thermography
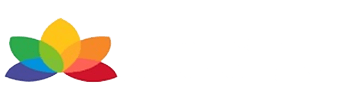
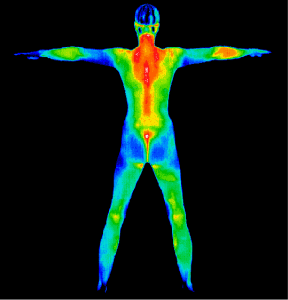
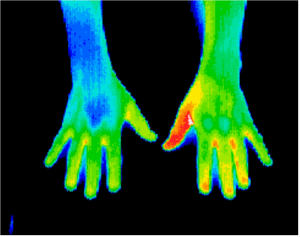
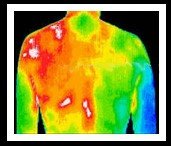
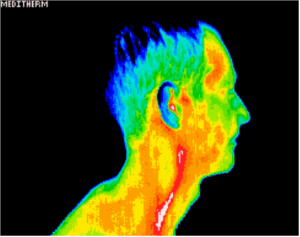
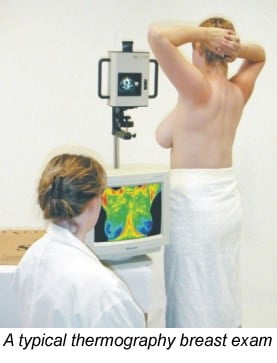
Clinical Thermography, otherwise known as Digital Infrared Imaging (DITI), is based on a careful analysis of skin and tissue temperatures. It is a diagnostic procedure that allows practitioners to see where there is abnormal chemical and blood vessel activity in body tissue. It is a non-intrusive procedure using the technology of the Infrared Camera and state of the art software.
With each scan an image is formed which is evaluated for signs of possible disease or injury. Extensive research and investigation performed at prestigious medical teaching institutions such as John Hopkins University Medical School, have established normal values for the distribution of heat in each region of the body. Variations from these normal values are measured and correlated with suspected injuries or diseases in the same way a blood or urine laboratory study is interpreted.
Over thirty years of clinical use and more than 800 peer-reviewed studies in medical literature have established thermography as a safe and effective means to examine the human body. It is FDA approved in the United States since 1982 and has been used there and in Europe for over twenty years. Thermography is a non-invasive test. It simply is creating an image of your breasts and body by measuring your heat. There is no contact of any kind, nor is there any pain or radiation.
According to IACT (International Academy of Clinical Thermology), breast thermography is a diagnostic procedure that images the breasts to aid in early detection of breast cancer. It is based on the principle that chemical and blood vessel activity in both pre-cancerous tissue and the area surrounding a developing breast cancer is typically always higher than in normal breast tissue. Since pre-cancerous and cancerous masses are highly metabolic tissues, they need an abundant supply of nutrients to maintain their growth and this can increase the surface temperature of the breast.
State of the art breast thermography uses ultra-sensitive infrared cameras and sophisticated computers to detect, analyze and produce high-resolution diagnostic images of these temperature and vascular changes.
By carefully examining changes in the temperature and blood vessels of the breast, signs of possible cancer or pre-cancerous cell growth may be detected up to 10 years prior to being discovered using any other procedure. This provides for the earliest possible detection of pre-cancerous and cancerous conditions.
According to IACT (International Academy of Clinical Thermology), breast thermography is a diagnostic procedure that images the breasts to aid in early detection of breast cancer. It is based on the principle that chemical and blood vessel activity in both pre-cancerous tissue and the area surrounding a developing breast cancer is typically always higher than in normal breast tissue. Since pre-cancerous and cancerous masses are highly metabolic tissues, they need an abundant supply of nutrients to maintain their growth and this can increase the surface temperature of the breast.
State of the art breast thermography uses ultra-sensitive infrared cameras and sophisticated computers to detect, analyze and produce high-resolution diagnostic images of these temperature and vascular changes.
By carefully examining changes in the temperature and blood vessels of the breast, signs of possible cancer or pre-cancerous cell growth may be detected up to 10 years prior to being discovered using any other procedure. This provides for the earliest possible detection of pre-cancerous and cancerous conditions.
No. Thermography, like mammography is a screening tool. Thermography identifies abnormal physiological changes in your breasts that may be cancerous. Mammography, a type of x-ray, identifies certain structures in the breast that can potentially be cancer. With both Mammography and Thermography, definitive diagnosis is done by other procedures such as a biopsy or lumpectomy.
Thermography does now have the ability to pinpoint the location of a tumor for biopsy purposes, thanks to new STI software. Consequently, for a comprehensive analysis, if indicated, an MRI ultrasound and/or mammography are recommended to complement breast thermography if breast cancer is suspected.
Current methods used to detect breast cancer depend primarily on the combination of both physical examination and mammography. While this approach has become the mainstay of early breast cancer detection, mortality from this disease has gone relatively unchanged for 40 years. Since the prevention of breast cancer has not become a reality as of yet, efforts must be directed at detecting breast cancer at its earliest stage, when there is the greatest potential for successful treatment. Consequently, the addition of breast thermography to the front line of early breast cancer detection brings a great deal of good news for women.
Because mammograms detect structural changes, a lump or mass of a size detectable on X-ray is already present in breast tissue by the time a problem is found. The next step is further investigation by ultrasound and/or biopsy to diagnose the nature of the lump or mass, and to make treatment decisions. At this point, it is often too late to implement preventive strategies alone and medical intervention is the norm or treatment.
In comparison, breast thermography detects functional changes in breast tissue before tumors form and when the tumors are too small to be detected with X-rays. This is done without radiation, compression, contact or needles. Unlike mammograms, thermography can be used for women of all ages and with all types of breast tissue: young, dense pregnant, breastfeeding, pre- and post-menopausal, fibrocystic, with breast implants, and when on HRT.
Because breast thermography is particularly useful during early phases of rapid tumor growth that is not yet detectable by clinical exam or mammograms, it has the potential to detect problems five to eight years before abnormalities can be seen with mammograms. This early detection of abnormal tissue activity makes breast thermography extremely useful and cost-effective as a screening strategy and gives the opportunity to apply non-invasive therapies to improve breast tissue function. The non-invasive nature of thermography also allows for repeat scans. This improves the ability to compare changes over time and monitor the results of preventive strategies to protect breast tissue.
- Unlike mammography and some other imaging modalities, thermography does not require radiation, compression, contact, or intravenous injection. As such, Digital Infrared Imaging is a very comfortable procedure which poses absolutely NO HEALTH RISK to the patient.
- While mammography relies primarily on finding the physical tumor, thermography is based on detecting new blood vessels and chemical changes associated with a tumor’s genesis and growth. By detecting minute variations in normal blood vessel activity, infrared imaging can frequently suggest a pre-cancerous state of the breast or the presence of an early tumor that is not yet large enough to be detected by physical examination or mammography.
- Difficulties in reading mammograms can occur in women who are on hormone replacement, are nursing, or have fibrocystic, large, dense, or enhanced breasts. These types of breast differences do not interfere with the thermography scans.
- Studies show that an abnormal thermographic image is the single most important marker of high risk for developing breast cancer-10 times more significant than a family history of the disease. Consequently, in the absence of other positive tests, an abnormal infrared image gives a woman an early warning. By maintaining close monitoring of her breast health with regular infrared imaging, breast self-exams, clinical examinations, and other tests, a woman has a much better chance of detecting cancer or pre-cancerous conditions at their earliest stage.
No not the moment.
Yes, hundreds of studies have been written up in medical journals.
No, a referral is not necessary.
The images are sent to Board Certified Clinical Thermologists for interpretation and you will receive your results/report and images within two days to two weeks depending on a few factors.
Full body thermography includes a breast scan, so is comprehensive. A full body thermogram which is suitable for both females and males, young and old, can identify pre-existing conditions, acute or chronic issues as serious as cancer, cardiovascular circulatory conditions, pre-stroke, nervous system disorders, repetitive strain injury, TMJ, arthritis, diabetes, melanoma, liver or kidney disease, thyroid disease, dental infections and, finally, breast cancer.
To ensure accurate thermal images, the following should be followed:
- On the day of your appointment, avoid using creams or other topical products on the breasts/body and any underarm antiperspirants or deodorants.
- Do not shave.
- Avoid exertion or exercise, hot tubs and saunas for at least 4 hours prior to your appointment.
- Avoid caffeine, nicotine gums, patches and tobacco products.
- No smoking at least 2 hours prior to your appointment.
- Avoid any stimulation to the breast/body a day prior to your appointment (no chiropractic, acupuncture, physical therapy, massage or use of hot or cold packs).
- If you are breastfeeding – wait 3 months for breast physiology to normalize.
- Avoid sun or tanning bed exposure to the breasts/body at least 5 days prior to the thermographic appointment.
- Please do not wear any scented products to appointments, including perfume, aftershave, scented deodorant, hair products or fabric scents as many of our clients are very sensitive.
A single breast scan gives information of the physiology of the body, on that specific day. It is advised to establish a baseline scan by repeating it in 3-6months time to see if any changes has occurred. Each woman has her own breast pattern (like a fingerprint) and the success and accuracy of Thermography relies on a follow up within the prescribed timeframe.
After that, the Thermal Imaging can be repeated annually or every second year.
Yes. Breast implants do not interfere with thermography. Breast Thermography is painless and safe, using no radiation or compression. It can be used effectively and safely for all women including pregnant or nursing women, women with dense breast tissue, and women with breast implants.
No. Breast thermography could give a warning signal in advance of invasive tumor growth. Combined with an unprecedented role in risk assessment, screening for younger women, and possibly prevention, breast thermography offers women information that no other procedure can provide. Mammography is used to confirm and locate the suspicious growth. A multi modal approach should be utilized, including breast self-examinations, physical breast exams by a doctor, thermography, mammography/ultrasound as required.
Your initial appointment will take 20 minutes for the breast thermography and 40 minutes for a full body thermography. During this time, you will complete the breast health questionnaire – and a detailed health history. You will then be taken to a private examination room where you will be asked to disrobe from the waist up for breast thermography and down to the underwear for a full body. This is to become acclimated to the temperature of the room. A female technician will be available to answer any questions. After 15 minutes, the technician will take a series of images including front, lateral, and oblique views of the breast including the underarm area and thyroid and, in full body, all images of the body.
You will receive your report and photo’s in an electronic format via e-mail within two days to two weeks. Other arrangements can be made.
Do you know that 23% of all breast cancers occur in women under 49?
This is the most common cancer in women in this age group. Breast cancers in younger women are usually more aggressive and have poorer survival rates. Breast thermography offers younger women a sensitive non-invasive (no radiation and painless) addition to the irregular breast health check-ups beginning with baseline screening from age 25.
Women with a family history can be at greater risk, but 75% of women who get breast cancer have no family history of the disease. Regardless of your family history, if a thermogram is abnormal, you run a future risk of breast cancer that is 10 times higher than a first order family history of the disease. Thermography is the only technology to provide women with a future risk assessment. If discovered, certain thermographic risk markers can warn a woman that she needs to work with her practitioner to improve her breast health.
There are so many options available which range from Orthomolecular therapy to lifestyle adjustments.
Your Doctor or Health care practitioner can explain all the option available to you for further management. Should your report show a cause for concern, please contact us to supply you with the necessary information.
How to prepare for your Thermogram
You must wait at least 3 months after:
Major breast surgery, completion of chemotherapy, or radiation before a thermal exam.
Please wait at least 1 month after biopsy or minor surgery
Avoid tanning or sunburn for 1 week before the examination
For 24 hours before the exam:
1. Avoid exercise or physical stimulation, massage, or chiropractic
adjustments
2. Refrain from sauna, steam-room, or hot/cold packs
3. No significant fevers
For 2 hours before the exam:
1. Refrain from tobacco use, coffee, or tea consumption
2. Please do not chew chewing gum.
3. Refrain from exercise, bathing, or shower
Scanning Process
A thermal scan takes approximately 20 — 45 minutes depending on which part of the body is being scanned. You will remove all jewelry and clothes from the part of the body being scanned. For a breast scan, you will be asked to disrobe from the waist up. While filling out the forms the surface temperature for your body will be allowed to equilibrate with the room. A female Technician will be performing all the imaging.
If you have copies of any other test results (e.g., mammograms, ultrasounds, biopsies) please bring them with you. If you have any further questions, please contact me.
Your images will be interpreted by a Thermologist, these are medical doctors trained to interpret the thermal patterns.
You will receive your report within a few days to a week after the scan.